By Kora Behrens, Clinical Nurse Manager, Medical Solutions
One of the most underrated skills that nurses possess is delegation. This skill is so very important to providing quality care in the healthcare environment. Furthermore, it has an even bigger impact as time moves on and the nursing shortage grows. More than ever, nurses need to work effectively to utilize their resources and assistive personnel. Proficient delegation is not always taught and it can be hard to master. It’s now more important than ever to have competent and appropriately supervised personnel in the delivery of affordable, quality care.
To achieve this outcome, the RN must assign tasks based on the needs and conditions of the patient, potential for harm, stability of the patient’s condition, complexity of the task, predictability of outcomes, abilities of the staff to whom the task is delegated to, and the context of the patient’s needs. One of the biggest rules to abide by with delegation that many nurses are not aware of are the five rights of delegation. These five rights include:
- The right task
- Under the right circumstances
- To the right person
- With the right directions and communication
- Under the right supervision and evaluation
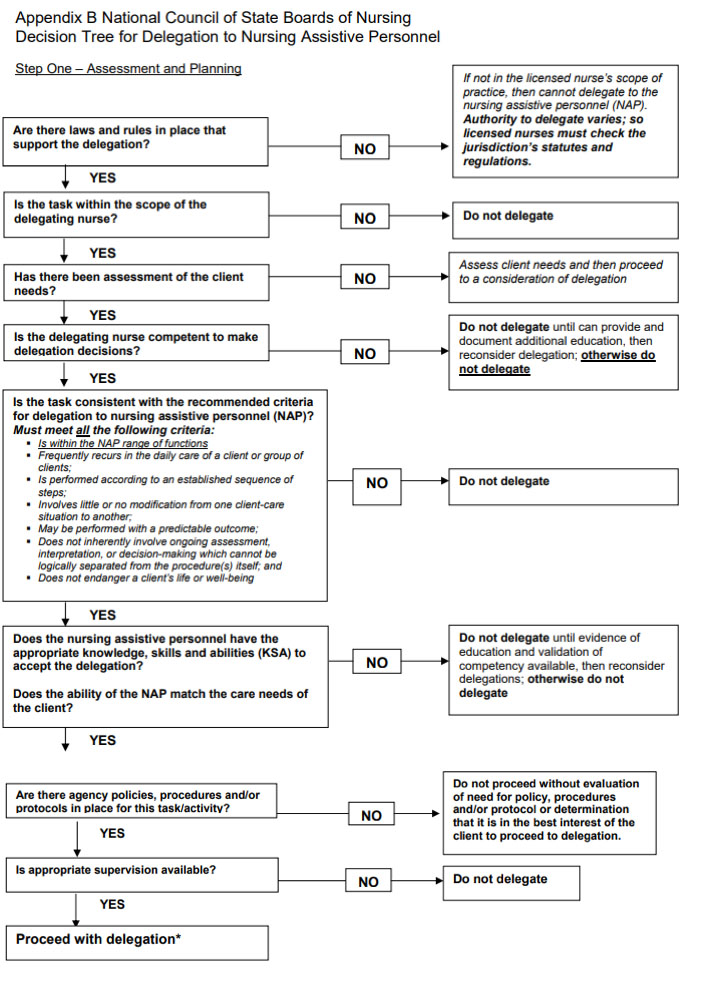
When following the five rights of delegation, nurses must use good critical thinking and professional judgment. Please refer to the following decision tree for assistance with delegation:
To assign a task to assistive personnel, the right communication must also occur to make sure directions are clear, concise, correct, and complete. The nurse must also assess the comprehension of the assistive personnel. To assess their understanding the nurse should ask how they will accomplish the task and when or how the information should be reported. The nurse should also determine what the assistive personnel’s expectations are and provide any clarification, as needed. In addition, the nurse should pursue the role of teacher provide guidance and support to the assistant.
Once the nurse has delegated a task to the assistant it is then his/her responsibility to monitor their performance and ensure that it meets the standards of practice as well as policy and procedures within the facility. This is the hardest portion of delegation as a Travel Nurse. Knowing all of the different equipment as well as policies and procedures is one thing, but to know the skill level of all assistive personnel and whether or not they are compliant with policies and procedures of the facility is even more challenging. The important thing to know as a Traveler is that diligent follow up is needed. Patients should be monitored frequently, but the nurse should also follow up with the assistant to determine areas of difficulty or gaps in comprehension.
The last and perhaps the most important part of delegation is feedback. The nurse should take a moment to reflect on all delegation to determine areas of difficulty and areas of strength. This will help tremendously in continuing to delegate and adjusting overall patient care according to changes or learning needs. This step is often overlooked or forgotten, and it is crucial to for nurses to evaluate the effectiveness in their delegation skills. Evaluation leads to development and this equates to better delegation which ultimately leads to improvement in patient care!